Sepsis & Infectious Diseases
Aims for the Week
Recognise the septic patient and list the SIRS criteria
Investigate the patient with sepsis of unknown origin
Institute the initial management with the 'sepsis 6' and explain the importance of its early delivery
Describe the appropriate use of antimicrobial agents
Correctly obtain blood cultures using an aseptic technique
Discuss the investigations and management of orthopaedic infections
Apply the local guidelines for the management of patients exposed to blood borne viruses including needlestick injuries
Initiate early management of Meningitis
List the differential diagnosis of fever in the returning traveller
Describe the course of HIV and its associated complications
Sepsis
Patients with infections are some of the most common presentations to the Emergency Department with some suitable for discharge home and others requiring aggressive resuscitation and HDU/ITU management.
Firstly, we need to know our definitions and basic treatment of sepsis.
The elderly or immunocompromised patients may not present with the typical septic response, however they may still be very unwell. Remember to consider sepsis in the elderly patient who is non-specifically unwell or who presents with delirium. These patients may deteriorate rapidly despite, reassuringly, appearing well on initial presentation. A great EM Docs blog discusses some of these issues and provides tips on how not to miss sepsis.
Antibiotics
Get to know your local hospital's antimicrobial guidelines.
Please also revise how to take blood cultures to minimise false positives.
Also, check out these summaries of the major classes of antibiotics:
Aminoglycosides
Beta Lactams
Macrolides
Emergency Infections
Meningitis is a serious infection that requires prompt treatment to prevent mortality. There are a number of excellent resources to guide treatment.
Necrotising fasciitis is an important and easy to miss soft tissue infection. This excellent video from EM in 5 will help you spot and treat it.
Blood Borne Viruses
The emergency department is often the first port of call for those with potential exposure to blood borne viruses whether by needlestick, sexual exposure, or through exposure to other body fluids. Knowing which patients need post-exposure prophylaxis for HIV or immunisation for hepatitis B is very important. Have a look at your local guideline to become familiar with what is required.
An Overview of Antiretrovirals
HIV Drug Interactions: This website has great factsheets on antiretrovirals and an interaction checker which will tell you whether an antiretroviral interacts with a patient’s medication (highly recommended).
Please note that when starting PEP you must alert the infectious diseases team (or GUM service post sexual exposure) to allow them to arrange follow up for the patient.
The Returning Traveller
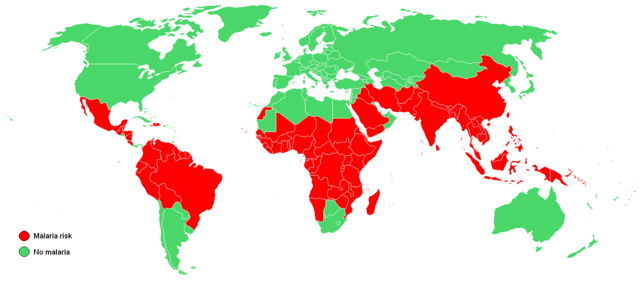
Fever in the returning traveller is an important (and vast) topic in infectious diseases that many of us are a little unfamiliar with, but may be presented with in ED. For this reason we wanted to revise some of the more important causes and their geographical distribution.
Revise history taking in fever in the returning traveller.
This map will give you an idea of which conditions you must consider in travellers from different parts of the globe.
Check out a brief overview of malaria, dengue and enteric fever.
Review this flowchart for diagnosing viral haemorrhagic fever in returning travellers and the RCEM guidance on ebola for emergency departments.
Wikipedia Creative Commons
There is extensive information on this topic on Travax (free registration with an NHS email address as long as practicing in Scotland) and also on Fitfortravel, which also provides good information for patients on diseases and prevention.