Episode 7: Dental Emergencies Part 1
Author: Eoghan Colgan @eoghan_colgan
Special Guest: Christine Goodall. @MAVScotland
21/2/2018
Listen
Guest Bios
christine goodall @MAVScotland
Christine is an Honorary Consultant and Senior Clinical Lecturer in Oral Surgery and Sedation at the University of Glasgow/NHSGGC and has been there for the past 14 years. Most of her training is in OMFS and she worked in various hospitals around Glasgow during her SHO years including the old Victoria Infirmary and Monklands moving on to do StR training in Academic OMFS in Glasgow and Aberdeen. She now works at Glasgow Dental Hospital and School where she divides her time between clinical work, research (she is leading on the evaluation of Navigator), teaching and running Medics against Violence a charity she set up in 2008. She is the Lead Clinician for her specialty, TPD for the West of Scotland and the Chair of the SAC in Oral Surgery (there aren’t that many oral surgeons!!). Years of nights spent running between EDs in Glasgow and Lanarkshire on a very old and now defunct SHO on call rota have given her invaluable experience in the management of dental and OMFS emergencies. These are some of the things she finds useful.
If you are in Glasgow and not sure of what to do please phone us. During the day you can get our triage nurse on 0141 211 9660 and quick access to a specialty grade oral surgeon for advice and help, from 5-9 you can call the GEDS (Glasgow Emergency Dental Service) service on 0141 232 6323 to access an experienced GDP and after 9pm you can call OMFS via the QEUH switchboard on 0141 201 1000.
Show Notes
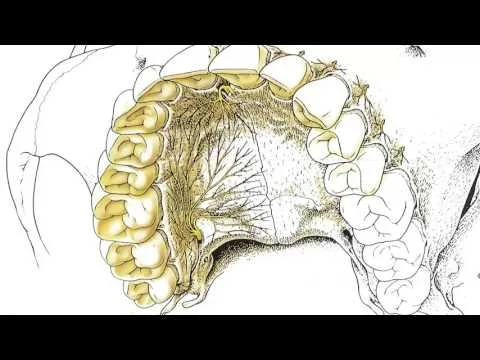
Eoghan interviews Dr Christine Goodall OBE on dental emergencies. Part one includes practical tips on how to manage post-extraction bleeds, dry sockets and facial abscesses secondary to dental infection. Many thanks to the Royal College of Physicians and Surgeons of Glasgow for loaning us the use of their fantastic new recording facility.
Take Home Points
Post –Extraction Bleed
(consider those which match your clinical skill)
Keep the patient relaxed
Swabs over bleeding and bite down for 20 minutes
Typically using dry swabs-anything you put in the mouth will end up damp after 20 minutes
Can consider adrenaline/tranexamic acid-soaked swabs if not settling
Local anaesthetic with adrenaline
Much better with dental syringe
Into buccal and lingual sulcus – avoid directly into gum
onsider Surgicel (particularly in those with coagulation problems)
Put small piece into socket then gauze on top and bite for another 20minutes
Suture the socket – buccal to lingual side – two stitches (can be criss-crossed) to close socket over (DISSOLVABLE if possible)
MOST stop – patience is required
Then don’t ‘fiddle’ with socket or rinse mouth for the rest of that day
Disposition:
If bleeding doesn’t stop – refer urgently to Max Fax if out of hours or your nearest oral surgery department during working hours
Those that stop may not require follow-up (and heal up normally) with regular follow-up as previously planned.
See dentist if any further problems
DRY SOCKET
Typically lack of clot formation after tooth extraction (visible bone within socket) causing significant pain. Not an infection but can get superinfected.
More common in the mandible, in women and in smokers
Infiltrate local anaesthetic around the socket in the buccal in lingual sulcus (non-attached musoca)
Lignocaine and adrenaline with dental syringe
Rinse with chorhexidine then irritate inside of socket with tweezers to encourage bleeding and clot formation
Apply pressure to control bleeding if heavy
If unable to anaesthetize (to facilitate irritation of the socket) – could pack socket with Alvogyl if available
Antibiotics not first line treatment but useful if the socket subsequently becomes infected usually due to food packing in the socket
Disposition:
If symptoms subside then see own dentist at next available working day
FACIAL SWELLING
Extraoral (if dental in origin they often have current or recent toothache)
Upper teeth – typically infraorbital, nasal/lip swelling. Typically from infection at canine or first premolar
Lower teeth: Submandibular, submental typically or if associated with a wisdom tooth submasseteric which may present without significant swelling but often presents with trismus.
Parapharyngeal and retropharyngeal are most worrisome and have risk of airway compromise
Typically they have signs of sepsis and often talk with ‘hot-potato’ mouth
Infection can track to mediastinum in worst case scenario
GumBoil – decay in tooth that got into root canal system and popped out on gum beside tooth (pimple)
Could consider antibiotics (amoxicillin or metronidazole)
Warm salty water may ‘draw out’ some of the infection
Paracetamol and ibuprofen best for toothache
Disposition:
Facial Swelling should be seen urgently by Maxillofacial, don't delay by sending to dentists or Oral Surgery as they need to be somewhere they can get to theatre urgently (particularly those with suspicious signs that suggest airway involvement). THINK ABOUT SIRS OR SEPSIS.
Gumboils should be seen by their own dentist on the next available day.