Slow Mo Major Incident
Author: David Chung, Vice President RCEM Scotland
4/1/18
I’m an Emergency Physician. My duty of care is not understood by many of my colleagues. I would say it is to be able to provide, at a moment's notice, the emergency treatment anybody in my catchment area might need, from a blue baby coming out of a car, to someone having a stroke or a heart attack.
Seemingly more mundane things are just as much our bread and butter, injuries, fractures, and mental and social crises are all stuff I take professional pride in dealing with well, by which I mean humanely, quickly, efficiently and safely.
For the past 2 weeks my Emergency Department has been struggling to do this. Our finite space has been asked to turn into a magical Tardis to solve the problems of increased demand, sicker patients and yes, the fact that large parts of the health and social care workforce have had 2 bank holiday weekends, if not an entire 2 weeks off. But it’s not magical, so it is full, too full to perform its primary duty of care.
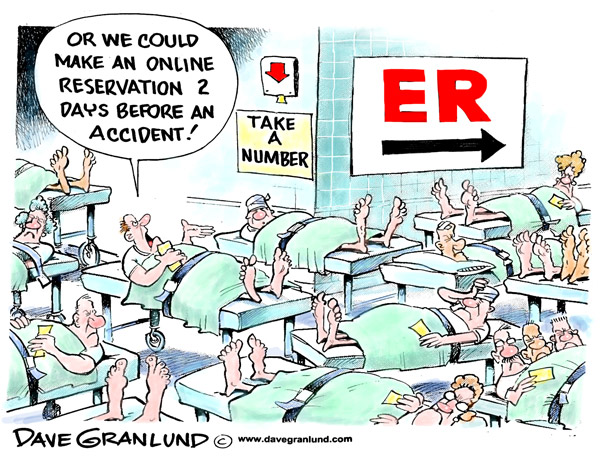
The Emergency Department is the only part of healthcare with complete open access open 24hrs a day. There is a mistaken assumption it will cope with anything thrown at it. That assumption is only held by those who don’t work there.
If you did, you would wonder how long old people could seriously be asked to go to a commode behind a curtain, in an 8 person observation bay , as they wait 16 hours to get to a proper ward and bed. You would wonder how, if there are 6 patients who need a high care (or Resuscitation room) space as opposed to a normal one, how are you going to put them into your resus room. You will be angry, because 3 of them should have been in a ward 6 hours ago. You will be worried you will end up resuscitating someone on the floor, as it is the only space.
As you come in on a morning to find your night shift looking shellshocked or in tears, you’ll give them a hug, metaphorical or physical and send them home. You’ll get into the 10 patients who have been waiting overnight and if you’re lucky you’ll spot the mistakes that have been made by overloaded staff and correct them without any harm occurring. Then you’ll hear management declare your department “safe”.
You’ll wonder if the patient who is terminal, and in their last hours will get the dignity of a side room to be with their family for the last few moments, or if, as has happened before, it’s going to be in a room with a drunk brought in by the police swearing next door.
You will also wonder why there are so few complaints from the patients and their relatives. Possibly there is a misplaced fear of retribution. When they do complain about these inhumane delays, they are often very the clear that the staff work like trojans and are not to be faulted.
The Emergency Department is a place with a finite capacity in space and time. It cannot be allowed to be congested because the only certainty is that more patients will arrive.
We are like the canary in the mine, or the Engine Fail light on the dashboard. If we’re in trouble, it’s because the entire health and social care system is failing. The causes are usually distant to us. The patients stuck in our corridors, waiting on a bed, or the “Exit Block” are usually due to delays downstream.
The care of acutely unwell patients is a continuous process, occurring seven days a week with predictable peaks and troughs. It’s like a busy restaurant, and to work well we need to simply staff it appropriately and clean as we go. What we have is akin to stopping washing up at your restaurant and 5, sending those staff home, and asking the chefs to do it, and the waiting because “ they’re there anyway”. Then there is an outcry after there weren’t enough plates clean and no one could get served.
But unfortunately, it’s more serious than a snappy analogy. It has been proven worldwide that Exit Block is harmful, patients in such a badly blocked system will encounter harm, and yes avoidable mortality.
This system is like Mid Staffs writ large across the whole UK. It’s like C Diff or MRSA, but for some reason it’s permitted. To solve it requires difficult questions about resources, and working practices to be asked. We need to, or we are complicit in avoidable harm.
Exit Block, and its causes are not unique to any system. They have been analysed worldwide and found to be consistent , whether you are in Glasgow, Sydney or Baltimore. The problems of long waits and ED crowding are found in all 4 Home Nations.
The causes are similar and extend beyond party politics, but the degree of system failure has been varied, with Scotland performing better and Northern Ireland being the worst. The resourcing of Health and Social Care across the UK as a whole does not provide enough to continue with a system that has a hope of performing safely.
This is a slow motion Major Incident, it needs to be treated like one. A whole system response.